Resuscitation Manual⁚ A Comprehensive Guide
This manual provides a structured approach to resuscitation, encompassing BLS and ALS guidelines, pediatric and neonatal considerations, and specialized techniques for challenging environments. It integrates evidence-based protocols from ERC and ILCOR, emphasizing practical application and technological advancements like the LUCAS device. Post-resuscitation care and long-term effects are also addressed.
Resuscitation manuals serve as indispensable guides for healthcare professionals and first responders, providing structured protocols and algorithms for managing life-threatening emergencies. These manuals synthesize current scientific evidence and best practices to ensure consistent and effective interventions. They typically cover a wide spectrum of resuscitation scenarios, encompassing basic life support (BLS), advanced life support (ALS), and specialized techniques for pediatric and neonatal patients. The organization and presentation of information within these manuals are crucial for efficient knowledge retrieval under pressure. Clear, concise instructions, often accompanied by visual aids, are essential for facilitating rapid decision-making in time-critical situations. Different manuals cater to various levels of expertise, from basic first aid to advanced medical procedures, ensuring accessibility and relevance across the healthcare continuum. The evolution of resuscitation techniques and technology necessitates frequent updates to maintain alignment with the latest scientific advancements and improve patient outcomes. The goal is to equip individuals with the necessary knowledge and skills to effectively respond to emergencies and maximize survival rates. Access to high-quality, regularly updated resuscitation manuals is critical for maintaining a high standard of care. These manuals are not merely collections of instructions, but essential tools for improving healthcare delivery and saving lives.
Key Guidelines and Protocols⁚ ERC and ILCOR
The European Resuscitation Council (ERC) and the International Liaison Committee on Resuscitation (ILCOR) are pivotal in establishing global standards for resuscitation practices. ERC guidelines, tailored to European contexts, emphasize ease of teaching and learning while adhering to rigorous scientific evidence. They provide detailed instructions for various resuscitation scenarios, reflecting the latest research and best practices. ILCOR, through its international collaborations, plays a crucial role in harmonizing resuscitation guidelines worldwide. Its consensus statements and recommendations form the basis for many national and regional guidelines, ensuring a consistent approach to life-saving interventions. Both organizations utilize a rigorous process to develop and update their guidelines, integrating scientific evidence with practical considerations. The emphasis is on creating clear, concise, and easily accessible documents that can be readily applied in diverse settings. These guidelines are not static; they are regularly reviewed and revised to reflect advancements in resuscitation science and technology. The collaboration between ERC and ILCOR ensures the global dissemination of evidence-based best practices, leading to improved patient outcomes and a more standardized approach to resuscitation across different healthcare systems. This unified approach is vital for improving the effectiveness of life-saving interventions worldwide.

Advanced Life Support (ALS) Guidelines
Advanced Life Support (ALS) guidelines, informed by the 2021 UK Resuscitation Guidelines and the 2020 ILCOR Consensus, provide a structured approach to managing complex resuscitation scenarios. These guidelines extend beyond basic life support (BLS), incorporating advanced airway management techniques, including endotracheal intubation and advanced airway devices. They emphasize the importance of rapid assessment and intervention, addressing critical conditions such as cardiac arrest, severe trauma, and respiratory failure. ALS protocols incorporate the use of medications, such as adrenaline and amiodarone, administered under strict guidelines. The guidelines stress the critical role of defibrillation, highlighting the use of automated external defibrillators (AEDs) and synchronized cardioversion. Monitoring techniques, such as electrocardiography (ECG) interpretation and pulse oximetry, are integral components of ALS, providing essential information for guiding treatment decisions. Regular updates to ALS guidelines are crucial, reflecting ongoing research and improvements in life-saving technologies. The integration of these guidelines with BLS techniques provides a comprehensive approach to resuscitation, significantly improving the chances of successful outcomes. Training and continuing education are essential for healthcare professionals to ensure competence in applying ALS protocols effectively and safely.
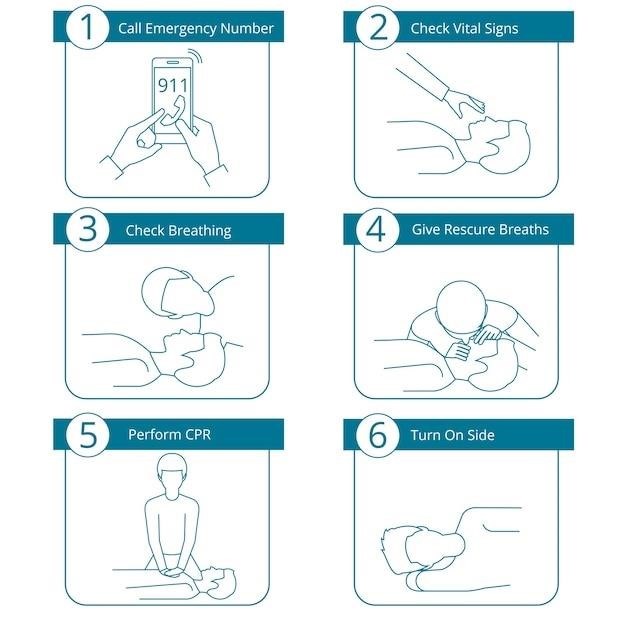
Basic Life Support (BLS) Guidelines⁚ A Step-by-Step Approach
Basic Life Support (BLS) forms the foundation of emergency resuscitation. The first step involves checking for responsiveness and activating the emergency response system (e.g., calling 911). Next, assessing for breathing and pulse is critical, determining the need for chest compressions. BLS guidelines emphasize the importance of high-quality chest compressions, delivered at the correct rate and depth, minimizing interruptions. The technique involves placing the heel of one hand on the center of the chest, interlacing fingers, and compressing the chest to a depth of at least 2 inches for adults. Rescue breaths, delivered after chest compressions, are essential to maintain oxygenation if the patient is not breathing normally. The ratio of compressions to breaths is typically 30⁚2 for adults. For infants and children, the technique is modified, with smaller compression depths and adjustments to the rescue breath delivery. Automated External Defibrillators (AEDs) are integrated into BLS protocols, aiming for rapid defibrillation in cases of cardiac arrest. BLS guidelines also stress the importance of teamwork and clear communication among rescuers, ensuring efficient and coordinated resuscitation efforts. Regular training and updates are paramount to ensure proficiency in BLS techniques, maximizing the chances of survival for victims of cardiac arrest or respiratory failure.
Chest Compressions and Rescue Breaths
Effective chest compressions are paramount in BLS. For adults, place the heel of one hand on the center of the chest, interlace fingers, and compress to a depth of at least 2 inches at a rate of 100-120 compressions per minute. Allow complete chest recoil after each compression to ensure adequate blood flow. Minimize interruptions to maintain consistent blood circulation. For children and infants, adjust compression depth and hand placement accordingly; utilize two fingers for infants and one or two hands for children, depending on size. Rescue breaths are crucial to provide oxygen. After 30 compressions, deliver two rescue breaths over one second each, ensuring adequate chest rise. For adults, use a mouth-to-mouth or bag-valve mask technique; for infants and children, use a mouth-to-mouth or bag-valve mask depending on the availability of equipment and rescuer comfort level. Proper technique ensures effective oxygen delivery to the lungs and the circulatory system. Regular practice and training are vital to ensure competency and confidence in performing chest compressions and rescue breaths correctly, maximizing the chances of survival for individuals in cardiac arrest or respiratory distress. Maintaining a consistent rhythm and depth is crucial for optimal resuscitation.
Airway Management Techniques
Effective airway management is critical during resuscitation. The initial step involves checking for airway obstruction; look for obvious impediments, such as vomit or foreign bodies. If an obstruction is present, carefully remove it using a finger sweep if visible. Head tilt-chin lift or jaw thrust maneuver is performed to open the airway; choose the appropriate technique based on the suspected cervical spine injury. For advanced airway management, consider oropharyngeal or nasopharyngeal airways to maintain patency. These airways prevent tongue obstruction, ensuring a clear path for air. Endotracheal intubation, performed by trained professionals, is the gold standard for securing the airway in critical situations. It involves inserting a tube into the trachea to deliver oxygen and ventilate the lungs. Proper technique is vital to prevent complications. Regular training and practice are essential for healthcare professionals to achieve proficiency in various airway management techniques. The selection of the most appropriate method depends on the patient’s condition and the rescuer’s expertise. Monitoring for effective ventilation and oxygen saturation is necessary throughout the process. Continual assessment and adjustment of airway management strategies are vital for successful resuscitation.
Automated External Defibrillator (AED) Use
Automated External Defibrillators (AEDs) are crucial in resuscitation, particularly for victims of sudden cardiac arrest. AEDs analyze the heart rhythm and deliver an electric shock if a shockable rhythm (ventricular fibrillation or pulseless ventricular tachycardia) is detected. Before using an AED, ensure the area is dry and the power is on. Turn on the device and follow the audio-visual prompts. Attach the electrodes to the patient’s bare chest, as indicated on the pads. Ensure proper placement to guarantee effective defibrillation. The AED will analyze the heart rhythm. If a shock is advised, ensure everyone is clear of the patient before pressing the shock button. After the shock, immediately resume CPR (chest compressions and rescue breaths) according to established guidelines. Continue CPR until the AED advises another shock or until emergency medical services arrive. AEDs are designed for ease of use, even by untrained personnel, making them invaluable in emergency situations. Regular training and familiarity with AED operation are vital for effective use. AEDs significantly improve survival rates when used correctly and promptly, making them an essential tool in resuscitation efforts. Always refer to the manufacturer’s instructions for specific operation details.
Neonatal Resuscitation⁚ Specialized Techniques
Neonatal resuscitation requires specialized techniques due to the unique physiological characteristics of newborns. Initial steps involve assessing the infant’s breathing, heart rate, and color immediately after birth. Gentle stimulation may be necessary to initiate spontaneous breathing. If the newborn is not breathing or has a heart rate below 100 beats per minute, positive pressure ventilation (PPV) with a bag-valve mask is initiated. Proper mask seal is crucial for effective ventilation. Oxygen supplementation may be necessary, but the concentration should be carefully monitored to avoid oxygen toxicity. Chest compressions are performed if the heart rate remains below 60 beats per minute despite PPV. The compression-to-ventilation ratio differs from adult CPR. Specialized equipment such as a neonatal resuscitation bag and appropriately sized endotracheal tubes are essential. Continuous monitoring of heart rate, oxygen saturation, and respiratory effort is vital. The use of medications such as epinephrine may be necessary in specific situations, always guided by established guidelines. Successful neonatal resuscitation often requires a coordinated team effort and adherence to established protocols.
Pediatric Resuscitation⁚ Age-Specific Considerations
Pediatric resuscitation differs significantly from adult resuscitation due to the unique physiological and anatomical characteristics of children. Age-specific considerations are crucial for effective intervention. Assessment should include a rapid evaluation of the child’s airway, breathing, and circulation. The approach to airway management varies depending on the child’s age and size. For infants, maintaining a patent airway often involves positioning and suctioning. Older children may require more advanced airway techniques. Bag-valve mask ventilation is commonly used, with careful attention paid to appropriate mask size and ventilation pressures. Chest compressions are performed if the child is pulseless or has inadequate spontaneous circulation. The compression-ventilation ratio and compression depth vary with age. The use of an automated external defibrillator (AED) is essential in pediatric cardiac arrest, with appropriate energy levels selected based on the child’s weight or age. Intravenous or intraosseous access may be necessary for medication administration. Effective pediatric resuscitation requires a thorough understanding of age-specific anatomy, physiology, and resuscitation techniques. Continuous monitoring and post-resuscitation care are crucial aspects of pediatric resuscitation.
Resuscitation in Special Settings (e.g., Tight Spaces)
Resuscitation in confined spaces presents unique challenges demanding modified techniques and careful consideration of environmental factors. Limited space restricts movement, hindering the implementation of standard procedures. Team coordination becomes paramount, requiring clear communication and efficient resource allocation within the constrained environment. Modified approaches to chest compressions may be necessary, adapting to the available space and the patient’s positioning. Airway management can be complicated by the lack of maneuverability. The use of specialized equipment, such as smaller-sized resuscitation bags or flexible suction catheters, might be essential. Maintaining a safe working environment for the rescuers is vital, ensuring adequate ventilation and preventing potential hazards. The presence of obstacles or hazardous materials necessitates extra precautions and potentially specialized personal protective equipment. Documentation of the resuscitation process, including the challenges posed by the environment, is crucial for post-incident review and improvement of future responses. Protocols should be tailored to the specific characteristics of the environment, ensuring the effectiveness of the resuscitation efforts while prioritizing the safety of both the patient and the rescuers.
The Resuscitation Crisis Manual (RCM)⁚ A Practical Approach
The Resuscitation Crisis Manual (RCM), inspired by aviation’s quick reference handbooks (QRH), offers a structured, two-page protocol format. The left page details immediate, life-stabilizing actions for crashing patients, prioritizing rapid intervention. The right page provides supplementary information and less critical steps, allowing for a tiered approach to crisis management. This design facilitates swift decision-making under pressure, mirroring the efficiency of cockpit procedures. Developed by experts, the RCM emphasizes a practical, readily accessible format to guide healthcare professionals through critical resuscitation events. Its step-by-step instructions and clear visual aids aid rapid comprehension and execution of essential procedures. The RCM’s checklist-like structure minimizes cognitive overload, ensuring a systematic and efficient response to urgent situations. This structured approach enhances team coordination, streamlining communication and actions during time-sensitive medical emergencies. The manual’s comprehensive coverage of major crisis scenarios makes it a valuable resource across various healthcare settings.
Utilizing Resuscitation Technology (e.g., LUCAS Device)
Modern resuscitation leverages technology to enhance effectiveness and efficiency. The LUCAS device, for example, is an automated chest compression system that provides consistent, high-quality CPR, minimizing rescuer fatigue and ensuring optimal blood circulation. This technology allows for uninterrupted chest compressions during critical procedures such as intubation or defibrillation, maximizing the chances of successful resuscitation. Integration of such devices into resuscitation protocols can significantly improve patient outcomes by maintaining consistent compression depth and rate, vital factors in cardiac arrest survival. Other technological advancements include advanced airway management devices and sophisticated monitoring equipment that provide real-time data on vital signs, aiding in prompt adjustments to the resuscitation strategy. Training in the use of these technologies is crucial for healthcare professionals, ensuring they can effectively integrate them into their resuscitation techniques. The incorporation of technology into resuscitation protocols represents a significant step towards improving the survival rates and long-term outcomes for patients experiencing cardiac arrest or other life-threatening conditions.
Post-Resuscitation Care and Long-Term Effects
Post-resuscitation care is critical for patient recovery and minimizing long-term complications. Immediate priorities include stabilizing vital signs, managing potential organ damage, and addressing any underlying conditions that contributed to the arrest. This often involves intensive care monitoring, mechanical ventilation, and medication to support organ function. Neurological assessment is paramount, as brain injury is a common consequence of cardiac arrest. Rehabilitation plays a crucial role in the long-term recovery process, addressing physical, cognitive, and emotional challenges. Patients may experience various long-term effects, including neurological deficits like memory loss, movement disorders, or cognitive impairments. The severity of these effects varies widely depending on the duration of the arrest, the extent of brain injury, and the effectiveness of post-resuscitation care. Ongoing monitoring and support are essential, and a multidisciplinary approach involving physicians, nurses, therapists, and support groups can significantly improve the quality of life for survivors. Psychological support for both patients and their families is also crucial in navigating the emotional challenges of this experience. Long-term follow-up helps detect and manage potential late-onset complications, optimizing the patient’s overall recovery and well-being.